Illustration by Julien Posture.
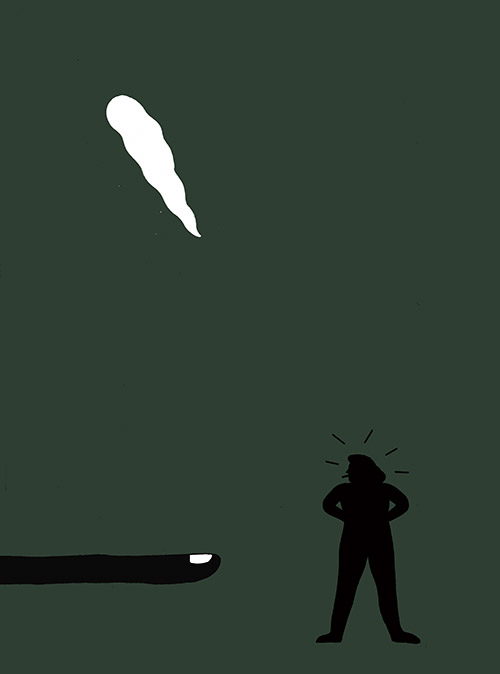
Illustration by Julien Posture.
Growing Pains
A tangled mess of cannabis laws is hanging Canadians out to dry and even endangering lives.
Early one morning in the summer of 2017, Eleanor Yu stepped outside her Montreal home to check her mail. As usual, the suburban street was quiet. Neighbours led their dogs down tree-lined roads before walking their children to school—that was the only traffic at that hour. Together with her two adult children, Yu owns another house just a short walk away, a duplex she was renting to two families.
As she sorted through her mail that day, one letter in particular caught her eye. The hydro bill for the rental units, where she covers the cost of utilities, had skyrocketed to five times the normal rate.
She brought it up with the downstairs tenants, and they immediately offered to pay the difference. It was a generous offer, but Yu was worried that it might be a malfunctioning heater, so she made an appointment with her electrician just in case.
While she waited, another odd thing arrived in the mail: an anonymous note from someone claiming to live near the duplex. They accused the same downstairs renters of running a marijuana grow op out of the basement. The writer described terrible smells wafting out of the house and of strangers coming and going at odd hours.
Yu had never had any problems with either of her tenants before, but now, unsettled, she had to think carefully about how to proceed. Growing marijuana for personal medical purposes has been legal in Canada for years, she knew—since 2001—and landlords are prohibited from asking about tenants’ health issues. More than that, she understood that some people need the drug to stay healthy, and that even she “might need it someday.”
Still, she had to do something. So, hoping to keep things civil between them, she invited the man living in the downstairs unit to her home for tea. When she asked him about the plants, he confirmed that he was growing four trees in the basement for his own personal use. They left it at that.
A month later, as the first snowfalls of the season were blanketing the roads, the electrician finally had time to check over the building in Notre-Dame-de-Grâce. The smell from the sidewalk should have been their first clue.
The tenant visibly panicked when they said they needed to enter the basement, and for good reason. After descending the staircase, they found not four but 244 cannabis plants lined up “like a vineyard” under heat lamps.
Unbeknownst to Yu (whose name has been changed, since her court case is ongoing), the tenant had knocked out sections of the wall for ventilation and had rewired the house. Thick red cables hung from the walls like warm licorice, terminating in a makeshift electrical panel dangling just inches away from the plants. The basement was a balmy 34 degrees in the middle of November. There was mould crawling across the ceiling.
The tenant pulled out a slip of paper, holding it up for the landlady to read. It was a licence from Health Canada granting him permission to grow cannabis for personal use.
Yu began investigating. Surely, she thought, even if the grow op was legal, the changes to her property were not, and someone must be responsible for the damages. She called the residential board of Quebec for clarification, but its hands were tied; she would have to call Health Canada. It was their license, after all. When she did, she was told that residential disputes weren’t their jurisdiction.
“I asked Health Canada if they have an inspector who could come, because I was really worried about the electrical and all that,” Yu said, “and they said no.” Her municipality had nothing useful to say, either, advising her to call the police. She never did get law enforcement involved; she didn’t want to further jeopardize her relationship with the tenant, and the police had already informed her that they can’t intervene if the tenant has a permit to grow.
Unwittingly, Yu had just stumbled straight into the medical-marijuana loophole—one of the many problems still plaguing Canada’s new legal cannabis system. According to federal cannabis regulations, medical license-holders like Yu’s tenant are under no obligation to inform their landlord if the grow site is their primary residence. They are even advised to “take measures so that other people do not know that you are growing marijuana,” such as limiting smells and visual clues from the outside. What’s more, the safeguards meant to ensure that these mounds of personal-use cannabis aren’t being sold on the black market are ineffectual, when applied at all.
Tucked in one corner of the hot, humid basement, next to the rows and rows of supposedly personal-use cannabis plants, sat a box of glossy business cards bearing the tenant’s name and phone number. The cards cheekily declared him, under a bright green marijuana leaf, to be a “Cannabiologist Specialist.”
In order to legally grow exactly 244 indoor plants for personal use, Yu’s tenant would have needed to obtain and submit a prescription for fifty grams of cannabis consumption a day. To put that into perspective, the pre-rolled joints sold at Quebec’s government-run cannabis stores typically contain half to one gram of dried cannabis each. Smoking fifty to one hundred of these joints a day would be incapacitating, if not impossible. Even Snoop Dogg, who once claimed to smoke “81 blunts a day,” might find cultivating an indoor farm more difficult under that level of influence.
A prescription for that amount only starts making more sense if the intent is to convert those fifty grams of dried cannabis into edibles or oils. The amounts required to make these vary enormously depending on method of extraction. About one cup of cannabutter, for example, can take up to ten grams of dried cannabis to make, while a full thirty-millilitre bottle of oil at a Quebec cannabis store—which uses an eyedropper to calculate dosage amounts—is considered equivalent to just six grams.
Health Canada doesn’t provide any standard conversion rates for these alternatives, despite being the authority that approves personal-use growing licenses. In fact, one of the reasons edibles won’t be federally legal to sell until October (a full year after legalization) is that the government initially deemed them too complicated to regulate. “It’s a complex area with a greater risk,” Bill Blair, the Liberal cabinet minister in charge of cannabis, told media in January.
Individuals are allowed to grow as many plants as their prescription deems necessary, with no hard limit. The onus of understanding particular methods of extraction falls on the doctors and nurses who prescribe cannabis as medication.
“Health Canada’s position is that a patient and their health care practitioner are best placed to determine whether or not cannabis is appropriate for the patient,” the agency wrote in a statement to Maisonneuve, “and Health Canada does not interfere in this process.” The agency does have an online info packet that patients can share with their health care providers to help them “make informed decisions about the benefits and risks of using cannabis for medical purposes.” But it doesn’t contain any specific dosing information for edibles.
Even if it did, patients need not go through the trouble of convincing their regular doctor to prescribe them that amount. Buying a prescription for fifty grams of daily consumption online is laughably easy. Websites like licencetogrow.ca offer a paid prescription service, allowing clients to pay for the dosage they want prescribed before they’ve even spoken with a doctor—which is illegal in Canada. The fee varies based on the number of plants the client wants to grow; for $800, their highest tier, the company will guarantee a prescription of fifty grams a day. The business even boasts a short appointment time, just two to three minutes over Skype.
With a copy of your prescription from a licensed medical professional, all that’s left to do is mail in a Health Canada form verifying your eligibility. If approved, the government will send you a certificate. Though Health Canada reserves the right to revoke your license if you violate their policies, there is no process for verifying or inspecting the grow site beforehand, and very little to no follow-up.
This is in stark contrast to the months-long (and much bemoaned) approval process for licensed producers who wish to officially grow medical or recreational marijuana for resale on the legal market. LPs, as they’re called, are required to have a fully built site at the time of their application, which is then reviewed in detail by the federal government and approved by the municipality before production can begin.
Over the years, Canada has increasingly billed its move towards legal weed as a public health effort. The medical cannabis system exists, of course, to provide a form of medicine to those who need it, and the Trudeau government framed the legalization of recreational marijuana last year as a similarly benevolent act. By legalizing cannabis, the government argued, they would be taking the industry out of the hands of criminals, making the product safer, and making it harder for young people to get the drug. But a year after legalization, the system is full of ambiguities and contradictions, a haphazard mess wreaking havoc on Canadians’ health and safety.
Norfolk County, in southern Ontario, is mostly farmland. Nestled between Hamilton and London, its fields are dotted with old greenhouses and divided by long stretches of road. The warm-for-Canada climate makes for prime agricultural real estate, and this, combined with the cheap price of land, has attracted a disproportionate number of personal-use grow ops.
When Greg and Laura France moved to Norfolk County in 2016 with their two-year-old son and baby girl, they didn’t know any of this. They chose a house close to Greg’s mother, directly opposite a tomato greenhouse where Greg used to work as a teenager. The neighbours brought over a flat of fresh tomatoes as a gift, and the Frances began fixing up their dream home.
A few months later, the greenhouse was sold to new owners. The new neighbours seemed friendly enough—they were a small group that kept to themselves. When Greg started hearing rumours that they were growing pot, he ventured over to say hello. Sure enough, he spotted a few cannabis plants sticking up from behind the remaining tomatoes. They joked about it good-naturedly, and Greg went home.
It wasn’t until a couple of months later that the pungent smell of marijuana began invading the Frances’ home, just sixty-eight metres away. The number of plants kept increasing, and it got progressively worse until finally becoming unbearable. The Frances’ eighteen-month-old daughter started waking up in the middle of the night, coughing and gagging.
The family picked up and left, finding refuge in Greg’s mother’s basement. These “forced migrations” became a regular occurrence, sometimes driving them to hotels and lasting up to a month at a time. “It’s this constant cycle,” Greg says. “You’re always at the mercy of the wind. You’re at the mercy of whatever they’re doing.”
The trend in the area is exactly this: old greenhouses are snapped up and repurposed for massive operations. Grow sites can be shared, according to federal regulations, by up to four prescription-holders in order to keep costs down. This has resulted in some personal-use facilities with over a thousand plants at a time, often in decades-old hothouses that have extremely poor air quality control, if any at all.
Every time Greg tried to confront the growers, he recalls, they would laugh and suggest he buy incense, repeatedly insisting that they had a license from Health Canada. When the Frances turned to the county for help, federal privacy laws barred the municipality from verifying the growers’ medical records.
It wasn’t until a warm afternoon in June 2017 that the Frances learned the truth. Police pulled up to the neighbours’ property and raided the grow site, seizing $3.9 million worth of marijuana and arresting seven people. By that point, there were more than five thousand plants in the greenhouse. And the neighbours didn’t, in fact, have a medical license to grow. The cops took away the plants and charged seven people with marijuana production and trafficking.
“We thought that was it. The nightmare was over,” says Greg. Not so. Within a month, a few of the same neighbours had returned. They hooked up a generator and began growing again, this time with an actual license from Health Canada. With it, they’re currently allowed to grow 1,356 plants for four people—or sixty-nine grams of cannabis a day per person—on the site of a multi-million-dollar drug bust.
These days, the stench is inescapable when the wind blows in the Frances’ direction. It soaks into their clothes and creeps in through closed windows. Laura started getting night tremors and constant, debilitating migraines. “Prior to that, I would maybe get six a year that were mostly weather-related,” she says. Now she gets headaches and migraines twenty days out of the month and has had to stop her work as a museum interpreter, since it involves lights and sounds that can be unbearable. “I worry about getting to the point where I can do my job again,” she says. “I’m not even myself anymore.”
They’ve barely opened their windows in two of the three years since they bought the house. “When the stink is hitting,” says Laura, “you can taste it.” And it’s not just the smell. Trucks and cars will come to the site at all hours, driving over the Frances’ property and laying on the horn. The greenhouse itself also makes a lot of noise, with fans, lights and alarms working constantly. Their calls to Health Canada have been fruitless, except to confirm the fact that the residents at that address have a valid personal-use license.
When I asked the Frances why they haven’t moved away, the answer was simple: they can’t afford to. “I want to leave in the worst way, but there’s no way we’re going to get anything even close to what we put into it,” Greg says. As property values in the surrounding area have gone up in the last few years, anyone trying to sell in the vicinity of the grow op has seen their properties languish, unsold.
The city planner for Norfolk County, Mat Vaughan, estimates that the region has about fifty such personal-use medical cannabis facilities, with more on the way. According to Health Canada records, Ontario was home to 4,102 personal-use licence-holders in 2017—the highest number in the country—beating out BC’s total by nearly a quarter. The number of personal-use licences granted in western Ontario alone was 857.
“There’s quite a few people living around them,” Vaughan says. “And there’s a big difference between living beside a greenhouse growing tomatoes and living beside a greenhouse growing cannabis.”
This is in part due to the fact that most of these old greenhouses have no odour, air treatment or light control, and incorporating these modern systems would be prohibitively expensive. An effective ventilation system for controlling odour, for instance, is about $40 per square metre. Greenhouse lights may not be as hazardous, but according to Vaughan, if proper blackout curtains aren’t installed then the lights used at night to maximize cannabis production make it “like living next to a football stadium.”
In the area around nearby Kingsville, population twenty-one thousand, licensed producers and personal-use facilities fill the sky with eerily bright lights, sometimes purple or orange, creating a sort of permanent borealis effect. Kingsville resident Nigel Lucas, who lives near a greenhouse, told me that he can read by the light at midnight and that “streetlights are obsolete.”
“We are in favour of the benefits the industry brings to the community,” he said. “But the lights can give the effect of the northern lights, where the midnight sun never sets.”
Hundreds of disgruntled residents turned up at a town meeting to argue against more licensed producers moving in, despite the boom in local jobs (around a hundred positions to build three commercial facilities). As a result, there are a lot of strict new municipal requirements on LPs, which now have to go through about six different light- and air-quality inspections just to get through the first stage of licensing in Kingsville.
But those, again, are just for licensed producers. There’s nothing either town can do to control the dozens of personal-use facilities, in part because neither the federal government nor the growers themselves are under any obligation to inform the town before they set up shop. And once a facility goes up, it can take years for a municipality to enforce its own bylaws. First, it can levy fines, and if that doesn’t work it can try to sue the homeowner—a costly and time-consuming process.
“Another one could pop up tomorrow and we won’t know about it,” says Kingsville Mayor Nelson Santos. “There’s no site-plan requirements, no setback requirements, nothing that allows us or gives us the opportunity to give input before they start building or put something up.”
When they do discover a new site, it’s often because of the facility’s foreboding security. “You can’t miss it,” says Santos, who recalls one barbed-wire fence going up in the middle of a residential area, right at the entry to Kingsville. “It looked like you were entering a penitentiary, a total compound all the way around.”
This security requirement at personal-use facilities and LPs is in place for good reason. These grow ops make for tempting targets for robbery, bringing an increase in crime to the surrounding communities. In late 2018, the Frances learned of an armed robbery at another personal-use grow op just down the road. Four men with handguns had broken into a grower’s residence in the middle of the night, assaulting and restraining the occupants before smuggling out a bunch of marijuana. Police arrested them eight hours later after setting up a highway blockade.
At the Frances’ home, there’s nothing but a wooden fence between them and the greenhouse across the street. And in Yu’s stiflingly hot Montreal duplex, another family with two school-age children used to live directly above. They had no say over what safety precautions their downstairs neighbours were taking against potential break-ins, if any.
Reaching solutions is painfully slow. Norfolk County is currently embroiled in a legal battle with the Frances’ neighbours—according to a new bylaw, the facility should be at least three hundred metres away from any other residences, which is more than four times its current distance. The growers, after attempting to amend that bylaw, are now taking an appeal to a provincial land tribunal. Until the province makes its final decision—which could take months—the grow op is free to continue operations.
In fact, things seem to be getting worse, not better. In late 2017, the county began to notice that some prescription grow ops, including the one across from the Frances, were doubling and tripling in size. These were on large parcels of land, some big enough to have two or three extra roadside entrances. It turned out that the prescription growers were using the addresses associated with those entrances to fool Health Canada into granting additional growing licenses, packing eight or even twelve registered growers onto one site.
That trick could bring the potential number of legal plants per personal-growth facility closer to 4,500. The growers knew something the county was only just beginning to understand: the federal government isn’t conducting any inspections before approving an application. They don’t check the address or the building’s condition, and so long as a licensed health care practitioner signs off on the prescription, they will turn a blind eye to the number of plants.
In a written statement to Maisonneuve, Health Canada confirmed that the agency “does not require an inspection of individuals’ and designated producers’ sites before it issues a registration,” but that if they’re made aware of a problem, an inspector may be sent to confirm compliance. If non-compliance is found, Health Canada has “a range of enforcement tools at its disposal,” including reminding the growers of their legal obligations or cancelling their registration.
“I think the folks who are running [the facilities] know the system,” Mat Vaughan says. “They know the loopholes, they know there’s a grey area, and they’re exploiting it.”
The dangers here are worse than sleepless nights and migraines. For personal-use growers like Yu’s tenant or the Frances’ neighbours, de facto legal immunity extends to local health and fire safety bylaws, as two fire chiefs lamented in a detailed 2016 report to the federal Task Force on Cannabis Legalization. “Typical residential buildings are not designed for significant indoor plant production,” reads the report, which leans heavily on data found in a 2005 study of residential grow ops in Surrey.
Using a list of residences with exceptionally high power consumption (provided by BC Hydro), the city of Surrey was able to conduct independent inspections of 252 licensed sites. Over half of these sites had issues that “posed high or extreme safety risks due to wiring or other electrical modifications,” the report said. About 10 percent had to have their hydro service disconnected immediately for “posing extreme safety risks.”
In addition to electrical issues, these grow sites were often found to have undergone structural modifications, including “increasing the size of rooms, manipulating plumbing and drainage, and making alterations to increase air flow.” In Yu’s basement, these last three were achieved by knocking large holes through the walls. The study estimated that these modifications posed “significant structural risks” in about 72 percent of the operations. The report ultimately recommends discontinuing the practice of licensing home cultivation entirely.
In April 2018, thirteen years after those damning statistics were first published, a house fire at a personal-use grow op took the lives of two Surrey residents and hospitalized two others. It’s believed that the growers had rewired their home in order to use industrial heaters, and when these malfunctioned, the grow op went up in flames. Firefighters on the scene had no clue that about two hundred plants were being grown inside, or that they would need to bypass a fortified basement door in order to reach the two victims trapped below.
“We have no idea where they are, or what’s going on, or when it’s going on,” Surrey Fire Chief Len Garis told the Vancouver Sun at the time. “We’ve kind of lost faith in the licensing system, to be honest with you.”
Health Canada has said that sharing licensing information with fire departments and municipalities would violate Canadian privacy laws, but Garis, who has since retired, argues that if these operations aren’t properly inspected and regulated, the growers don’t just “bring about dangers to themselves,” but to others as well.
How could this loophole become so entrenched? In short, over many years and with many halting, patchwork steps. The enormously convoluted process of building our medical cannabis system from the ground up has left plenty of little cracks along the way.
Medical marijuana has been legal in Canada, to varying degrees, for almost two decades. Starting in 2001, patients with prescriptions were allowed to grow and store their own personal stock. Under the Harper government, in 2013, personal growing was banned entirely. Patients were instead required to buy from licensed distributors—at a significant mark-up. After this proved unpopular, and after the Federal Court objected to the law’s limitations, a hybrid of the two systems was created in 2016, under Trudeau.
On October 17, 2018, that medical system was absorbed into the Cannabis Act—a giant, wonky umbrella of new regulations now subdivided by province, but which continues to exempt medical marijuana from many oversights.
When I followed up with Garis, who co-wrote the 2016 report highlighting fire hazards, he was no more optimistic than he was three years ago. “I do not expect there will be many differences… in the new regulations for home grown,” he wrote to me. “Home buyers beware.”
When it comes to maintaining safe homes, property owners are the logical place to start. But even when they try to fight back against potentially dangerous changes to their property, the loss of their rights can be near-total within this legal quagmire. In Montreal, Yu’s tenant has since moved out of her building, but the damage is done. The mouldy, damaged unit remains unrentable until it’s fixed. And it’s still unclear, given the tangled mess of federal and municipal regulations, who should pay for those repairs. Yu says she “can’t deal with the headaches” and has stopped trying to get answers from the federal government.
“Once you have this problem in your building, it’s the end of the world,” said a spokesperson for the Quebec Landlords Corporation (CORPIQ) who is familiar with the severity of Yu’s case. Whoever buys Yu’s building will have the right to know that there was a grow op in the basement, and banks don’t like to finance these sites.
Neither do insurance companies. In February, the BC Superior Court ruled that home insurers don’t have to cover damages after a major house fire in cases where there was a grow op on site—even if the plants were being grown legally, and even if they weren’t the cause of the fire. The presence of even a single cannabis plant could be enough to deny a claim.
“More people than ever are getting these licenses,” the CORPIQ spokesperson told me. “It doesn’t take into account the huge responsibility of the homeowner. We need rulings that say, ‘We know you have a permit [to grow], but their home is not your own.’”
In agricultural towns, balancing the rights of farmers and homeowners shouldn’t be insurmountable. There’s a precedent: in the early 1970s, young urbanites in southern Ontario began seeking cheap housing in rural areas. Right around the same time, factory farming was becoming common practice nearby, bringing a sharp increase in odours and pollution. Manure production from livestock in Ontario was equivalent to a human population of over forty million, and the new human residents building their homes across the road began to take notice. With no regulatory regime in place, disputes between neighbours were handled ad hoc by the municipalities. “It was a mess,” says Mat Vaughan, until Ontario eventually adopted province-wide “Minimum Distance Separation” guidelines for livestock and residential areas and the public health crisis began to settle.
“We need something like that for the cannabis production process,” says Vaughan. “Strictly, at least, for mitigating land-use conflict.” But in this case, the federal government doesn’t give provinces and municipalities the chance to enforce any such regulations before issuing licenses. Robert Brown, Kingsville’s city planner, says so concisely: “Health Canada won’t give us the time of day.”
To anyone paying attention, it should be clear that a lot of this personal-use medical pot is being redistributed onto the black market. But shouldn’t that business be drying up with legalization?
Not at all. Statistics Canada recently found that 59 percent of respondents, nearly a year after legalization, are still purchasing their weed from illegal sources. This loyalty to the black market is due in part to the high cost of legal recreational weed—it’s been rising since October, to almost double that of illegal pot. The average price gap is nearly $5 a gram.
This isn’t just an abstract economic problem. For many medical cannabis users, it’s an urgent dilemma. One in four medical cannabis users reported having a harder time accessing the cannabis they need since recreational legalization, according to one study.
There are three reasons for that. First, before legalization, many medical cannabis users preferred buying cannabis at dispensaries they trusted rather than government-run programs. According to Rielle Capler, a cannabis researcher at the British Columbia Centre on Substance Use, distrust towards the government was a big factor. “They don’t want to have their name on a list, for example,” she said.
Second, many of those private dispensaries—which used to exist in a sort of legal grey zone, selling black-market weed—have either been shut down or forced to obtain an expensive provincial licence. And third, the government has been slow in granting new distribution and production licenses, and people in the field suspect that most of what’s produced goes to government-run stores first. The resulting shortages have been making international headlines since day one. Suddenly, last fall, medical users with legitimate needs had nowhere to purchase legal marijuana.
More than that, the available legal stock is often, well, very old. In BC, the provincial distributor overstocked on cannabis products ahead of legalization, but the government had yet to license enough dispensaries to sell it all. That means the provincial warehouse is “full of old products,” said Jeremy Jacob, president of the Association of Canadian Cannabis Retailers. The worry among those in the industry is that the provincial supplier will be “determined to sell these first.” Some medical cannabis users have reported receiving products over eleven months old—which are at best, stale, at worst, mouldy.
These incidents are especially aggravating for BC businesses, who pride themselves on their reputation for high-quality marijuana and dispensaries’ strict oversight. In 2015, Jacob co-founded a dispensary, The Village Bloomery, in Vancouver’s trendy Kitsilano neighborhood. The store opens onto a brightly lit courtyard, with the constant trickle of a fountain nearby.
Before legalization, The Village Bloomery relied on “grey” market producers, many of whom would have integrated into the new legal system if they could have—if the government had decided to allow “micro” licenses, a middle zone between the four-plant personal allotment and the industrial licenses that cost millions of dollars.
But what the government considers to be a micro operation is too tiny for most black-market growers to justify the cost of obtaining a license. “It’s no longer about whether you have skills or expertise,” said Jacob, “it’s more about do you have millions of dollars up front.” Had lawmakers made room for more small growers, it would have ensured a more consistent flow of stock from before to after legalization.
The loss of privately owned dispensaries is another looming headache for medical users. About half of the customers who frequent Anita Roy’s shop on Vancouver Island, for example, are senior citizens who come seeking alternatives to the powerful opioids and antidepressants they’ve been prescribed. Roy is a former property manager who got into the cannabis industry thinking it would be a fun way to spend her retirement. She started off working part-time at a retail cannabis store but gradually started taking on more hours as she grew to love the business. In 2017, she opened her own dispensary in Parksville, close to home. Her favourite part about selling cannabis is talking to clients.
“They go on pot and they’re like, ‘Wow!’ They can throw out those horrible medications that come with all the pharmaceutical side effects,” she says. “My entire business is based on personal relationships.”
Roy, like some other optimistic BC dispensary owners, has stayed open without a license in the hopes that the system’s current disorganization will shield her from any serious repercussions. The one time local law enforcement came to her door, the single police officer they sent “seemed embarrassed to be arresting an older woman” and the charges against her were dropped.
But that leniency won’t last forever. When the province finally decides to take small businesses like hers more seriously, which could happen any day, Roy will either have to close her doors or buy a license to distribute. If she decides to get a license, she’ll have to give up what she loves most about running a dispensary: giving clients information that could be construed as medical advice. Under the Cannabis Act, the only people allowed to advise on dosing are doctors, nurses and pharmacists.
“I don’t pretend to be a doctor, but I’ll say ‘This will really help you sleep. It helps in 99 percent of people,’” she says. “I won’t be able to do that in the new environment.”
This restriction is especially irksome given the lack of cannabis savvy she sees amongst medical professionals. She gave me an example of a client coming in with a doctor’s prescription for “two grams.” “Two grams of what?” she laughs. “Two grams of bud, flower, concentrate, two grams of edibles? It doesn’t make sense.”
Appropriate dosing, according to both Roy and Rielle Capler, has long been understood by dispensaries, built upon long-term relationships between dealers and clients. These are standards that go back decades, if not far longer.
“It’s like they’ve rolled us back twenty-five years,” said Jeremy Jacob. “And we feel that this is quite Orwellian—quite surreal that we can’t talk about the things that people want to talk about when they come into a cannabis shop for the first time.”
When I tell Roy about the prescriptions I’ve seen, in the range of fifty to two hundred grams, she’s not surprised. All her current stock comes from local growers with personal-use medical licenses, the kind of licence the growers in Norfolk County have. “A lot of people have been laughing their heads off because the government has no idea what they’re issuing licenses for,” she said. “It’s totally ludicrous; obviously it’s a commercial application.”
When the province starts sending out more than one embarrassed cop at a time, Roy will have to start buying stock from government suppliers—growers she’s never met. The licensed weed will be more expensive than her current supply and potentially quite old. The province is even setting a maximum resale price. The hit to her revenue will be painful, but Roy told me that, if she’d had the opportunity, she would have gladly worked with the government to comply with new regulations to ensure quality and safety. That, after all, is already a big part of her business. “People come back to us over and over again because we are so careful.” I can hear the exasperation in her voice. “Why would the government think that independent operators have no interest in safety?”
Considering the France family’s migraines and other health problems, the two men who died in Surrey, the mouldy products being sold in provincial stores and the neighbours who lived, oblivious, on the second floor of Yu’s sweltering, rewired duplex, one has to wonder if people’s health comes into the government’s equation at all.