 Illustration by Julia Kreutz
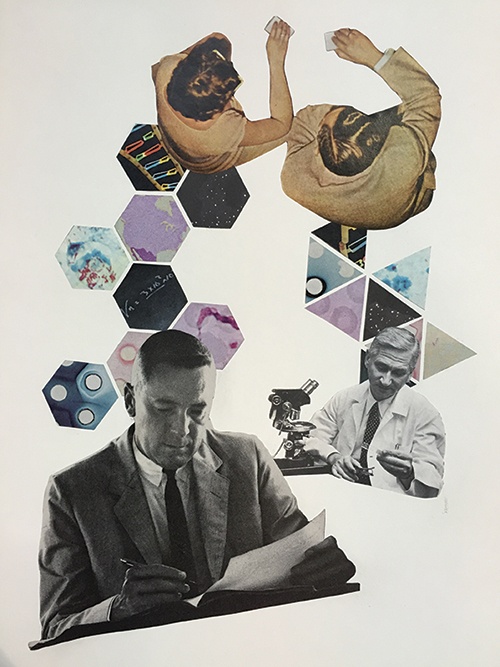
Illustration by Julia Kreutz
DNA Discrimination
Canada is one of the only countries where people can be marginalized due to their genetics. But that may soon change.
In the fall of 2008, during her fourth year at the Canadian Memorial Chiropractic College in Toronto, Dr. Anne Lakeland* listened carefully as a financial advisor delivered a talk about the need for life and disability insurance. The audience, all students in their final year, were told that they were excellent candidates for insurance—as long as they didn’t have any serious medical conditions.
The soon-to-be chiropractor was concerned: her father carries the genetic mutation responsible for Huntington’s disease, an inherited, often fatal brain disorder that leads to impaired motor and cognitive functions. Lakeland approached the financial advisor and asked whether her father’s condition would affect her applications. The advisor offered to make some anonymous inquiries on her behalf.
Lakeland was told that without life and disability insurance, she would be unable to set up a medical practice. So when the insurance companies told her intermediary that Lakeland needn’t apply—her family history rendered her ineligible—she was more than a little distressed. She could take a genetic test, but only a negative result would ensure her eligibility with any of the major insurance firms. “[It] was pretty devastating and very frustrating,” she recalls. “And certainly, you know, not what you want to hear when you’ve spent seven years in school.”
Canada has a notable distinction among G7 nations: it is the only country without laws protecting against genetic discrimination. What that means is that third parties can demand genetic tests and then discriminate against individuals based on their results. While this happens most often with insurance companies, it has occurred in other areas including employment, custody, adoption and even mortgage eligibility.
At the same time, the field of genomics has become increasingly medically useful. With a simple cheek swab, scientists can now diagnose and screen for heart disease, various cancers and even rare monogenic disorders such as Huntington’s.
Moreover, the science behind genomics has developed rapidly. In 2003, there were tests available to screen for about 100 genetic mutations. Now, we can screen for well over 48,000. As well, instead of running individualized tests for specific mutations, scientists can now use a shotgun-like approach to screen for thousands of diseases at once. As Dr. Ronald Cohn, a geneticist and the chief of paediatrics at SickKids Hospital explains, we’ll all be carrying a copy of our genomes in the not-so-distant future.
Despite these advancements, many Canadians are declining to get tested due to fear of how the results can affect their futures. Dr. Yvonne Bombard, a leading genetics health services researcher at St. Michael’s Hospital in Toronto, has conducted pioneering research in Canada on this subject. In one study, which surveyed participants at risk of developing Huntington’s disease, 40 percent reported experiencing genetic discrimination, mostly in social, familial and insurance settings. Cohn estimates that about 15 percent of the people he sees decline testing for this reason; it is “paralyzing,” he says, to be unable to provide the best care possible for no other reason than how it may affect a person’s insurance.
Not only that, insurance applications are stored in a single repository called the Medical Information Bureau, which insurers access when they evaluate prospective applicants. This means that biological kin can also be impacted by the results of a lone relative’s genetic test. Due to the lack of regulatory protection today, those who opt for testing thus expose not only themselves, but their entire family, to the consequences.
All of Canada's major political parties appear to largely agree on the need for legal protection against genetic discrimination. The Liberals promised to address the issue during the 2011 election, former NDP Member of Parliament Libby Davies introduced a private member’s bill barring genetic discrimination in October 2013, and later that same month, the Conservatives vowed to tackle the issue during their Speech from the Throne. But a mix of unfortunate timing, mundane parliamentary procedure and opposition from the insurance industry has held up meaningful results.
For their part, insurance firms claim that any new law will open the floodgates— in effect, that people will take out expensive policies immediately prior to getting a genetic test. But anti-discrimination laws already exist in all other G7 countries, where insurance firms still carry on; similarly, not many genetic disorders carry such a dire prognosis. “A number of disorders you can find out about—specifically as an adult—are medically actionable,” Cohn says.
Senator James Cowan, who has been researching and advocating for a genetic nondiscrimination law since late 2011, offers a cogent example. Suppose, he explains, two identical twins are at a heightened risk of heart disease. One takes a genetic test and changes their lifestyle by eating healthier, exercising more and quitting smoking. The other declines testing and maintains unhealthy habits. If the second twin dies at a young age, the insurance company gets stuck with a large life insurance bill. “Just to put it in pure economic terms, the longer you and I are healthy and pay our insurance premiums, the better off the insurance companies are,” Cowan says.
Beyond economic impacts, there are bigger societal issues at play. In Canada, legal provisions protect against discrimination based on race, gender, sexual identity, religion and other personal characteristics. Yet genetics—another aspect of our lives we have no control over—remain vulnerable. That’s why, when a comprehensive review of the Human Rights Act was under way in 1999, Senator Sheila Finestone noted that genetic discrimination could become the civil rights issue of the new millennium.
The political battle to bar genetic discrimination has been a long one. In the spring of 2013, Cowan introduced Bill S-218, an act to prohibit and prevent genetic discrimination. The bill would amend the Canadian Human Rights Act and the Canada Labour Code, as well as making it a criminal offence to require a genetic test.
Cowan consulted widely, meeting with advocacy groups, parliamentarians, insurance firms and other interested parties. But between April and September of 2013, debate on Cowan’s bill was adjourned repeatedly. It died when parliament was prorogued in September of that year. Cowan reintroduced the same bill (now called Bill S-201) the day after parliament returned. Again, debate was repeatedly delayed until the bill was referred in June 2014 to the Senate Committee on Human Rights. In February 2015, the Conservative majority on that committee voted to gut the bill, deleting eight of its eleven clauses. (Two of three preserved sections pertained to trivial matters, such as the bill’s short-title and defining “disclosure” and “genetic test.”)
The House Conservatives introduced their own bill in June 2015, but it contained weak provisions and offered no protection against individuals being required to take a genetic test. Because it was put forward only a few weeks before the 2015 summer recess and federal election that followed, it died, too.
After the Liberals were elected last year, Cowan reintroduced Bill S-201. It has already passed unanimously in the Senate and passed its second reading in the House this October. If it becomes law, Bill S-201 will go a long way to address the issue of genetic discrimination in Canada.
Anne Lakeland's story is one of the happier tales. She was eventually able to find a smaller insurance company—and a smaller policy—that only asked about her personal history. In turn, she declined testing. “I could very honestly say that I had no genetic or neurological or any other type of diseases,” she says.
But Huntington’s was still on her mind. Lakeland had been volunteering with the non-profit Huntington Society and her graduate research focused on the disease. About a year and a half after obtaining insurance, she finally decided to have a genetic test.
Lakeland was fortunate to find out that she was not a Huntington’s carrier. She was free thereafter to get a larger policy with any of the major Canadian insurance firms. Nonetheless, the process caused her considerable angst. Even with a negative result, she still struggled with the health, familial and emotional tolls of getting tested. “I knew that no matter how the results came back, my life was going to be forever changed,” she says. At the time, getting insurance should have been the least of Lakeland’s worries. But that wasn’t the case for her, and it still isn’t the case for many Canadians to this day.